How Long Does It Take For Fungal Acne To Clear

What is fungal acne?
Fungal acne (AKA Pityrosporum folliculitis or Malassezia folliculitis) looks a lot like hormonal acne or bacterial acne but is actually quite different. In fact, it's not even really acne at all! While bacteria cause regular acne, fungal acne is caused by an overgrowth of another abnormal skin flora—you guessed it—fungus!
This fungus "feeds" on oil on our skin either from our own skin's oil (sebum) or any other oils or oil-rich creams applied to the skin. For some people, this fungal infection results in a skin disorder called Tinea versicolor. In others, it causes an infection of the hair follicles that resembles traditional acne—acne-like red bumps with occasional whiteheads. In contrast to real acne, with which you may see many types of different acne lesions together (some blackheads, some papules, some cysts), in fungal acne, there is a uniform appearance to the bumps...and they are frequently itchy!
Where is fungal acne located?
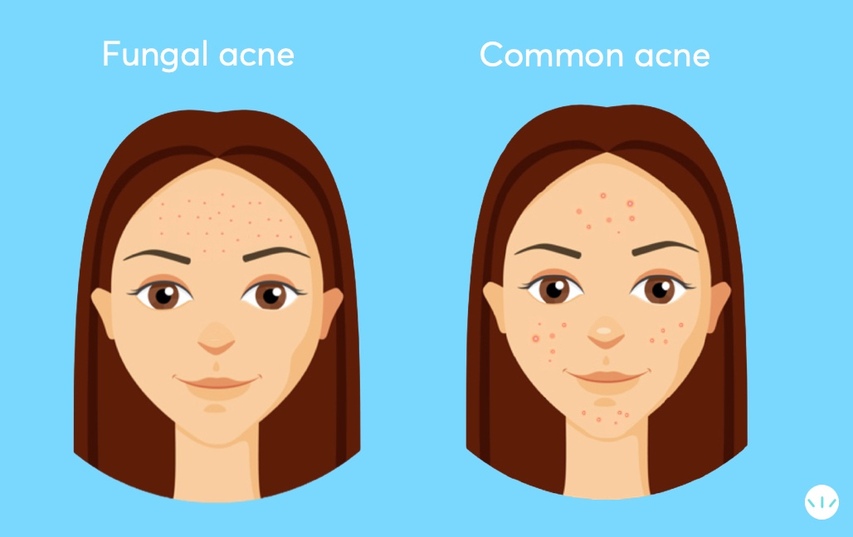
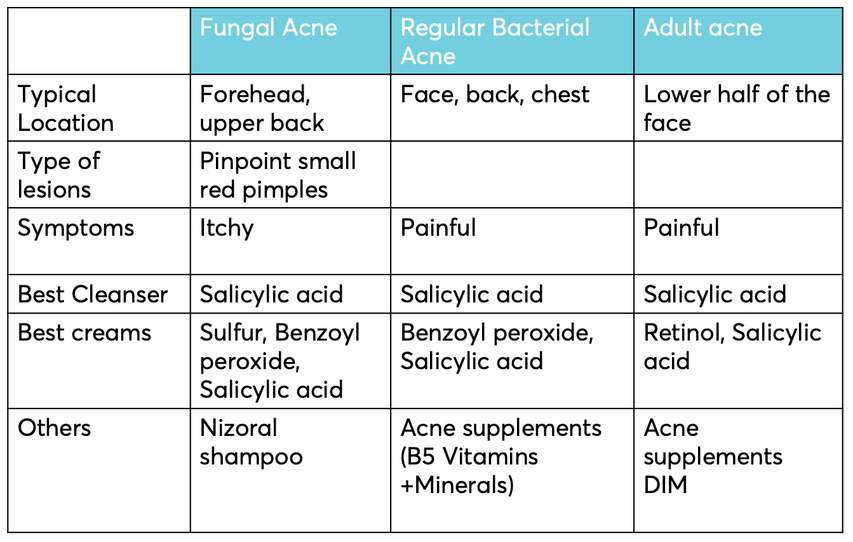
Because Pityrosporum and Malassezia fungi depend on oil for survival, fungal acne is most common in oil-rich areas of the face and body such as the forehead (t-zone), sides of the nose, chin and the upper back, chest, and shoulders. It can pop up in the same areas as traditional acne and seborrheic dermatitis and can even occur simultaneously. If you're not sure what skin condition you have, consult your local physician, or seek a dermatologist.

Pityrosporum folliculitis in a 34-year-old construction worker. The condition developed after working in a hot, humid environment for a few days. (Georgios Gaitanis et al. The Malassezia Genus in Skin and Systemic Diseases).
What is the best cleanser for people with fungal acne?
People with fungal acne should look for a cleanser that includes salicylic acid and green tea extracts. Salicylic acid is a keratolytic agent used for fungal skin infections. It causes exfoliation of the skin's stratum corneum layer, removing dead skin cells and fungi. Green tea is rich in catechins, antimicrobial and anti-fungal, and helps destroy bacteria and fungi spores. In one study, subjects with Malassezia infection underwent bath therapy using green tea extracts three times a week over four weeks. Results showed that all subjects experienced a significant reduction in their skin symptoms,
What causes fungal acne (Pityrosporum folliculitis)?
Our skin has its microbiome (i.e., immune system) with a balance of bacteria and yeast. The problem in both traditional acne and fungal acne is when something throws off this balance.
- Climate: Because yeast thrives in warm, humid places, fungal acne is more common in these types of climates and seasons. Interestingly, 56% of people with acne in the Philippines (hot and humid!) have both regular bacterial acne and fungal acne—a much higher rate than average!
-
Antibiotics: Long-term use of topical antibiotics such as clindamycin or oral antibiotics such as doxycycline and minocycline can make fungal acne worse. By killing off bacteria (both harmful and good!), antibiotics allow the fungi on the skin to proliferate. In a clinical study looking at people with fungal acne, six of the six cases were previously treated with topical or oral antibiotics. Two with clindamycin, 2 with erythromycin, and two with oral minocycline. This is another reason to avoid topical or oral antibiotics when treating acne. Better choices for treating common and fungal acne are benzoyl peroxide, salicylic acid, and retinol.
-
Hygiene: Did we mention yeast-like warm, humid environments? Does that ring a bell about any of the places you frequent...for instance, the gym? Starting a new exercise program, wearing the wrong workout clothes, and/or leaving sweaty garments on your body for too long can all lead to fungal acne and what's known as folliculitis.
-
Skincare Products: Did we also mention yeast feed on oil? If you're using skincare or makeup products that contain oil (even small amounts), it could be a trigger.
- Diet: While diet isn't typically the initial cause of a fungal acne outbreak, once there is an existing imbalance, your diet—is high in sugar (yeast's other favorite food!)—can certainly be a contributing factor!
-
Steroids: Taking oral corticosteroids, and especially prednisone, is another possible cause of fungal acne. (Pityrosporum folliculitis). Those fungal acne breakouts will usually start two weeks after one starts to take steroids. This type of steroid-induced acne can also be caused by steroid inhalations, bodybuilding hormones, and potent topical steroid cream used on the body's face for more extended periods. Steroid fungal acne will begin to subside once prednisone is discontinued. During prednisone treatment, effective topical treatment based on benzoyl peroxide and ketoconazole shampoo can control outbreaks.
-
COVID masks: If your fungal acne is on the lower parts of your face and around the mouth, it may be caused by your COVID face mask. The single-use surgical masks are made of polypropylene, a type of plastic that traps the humidity and heat under the mask. This environment provides excellent breeding conditions for bacteria and fungi and, in turn, increases the risk for regular and fungal acne. The best solution for this maskne is using a cotton mask impregnated with antibacterial/anti-fungal copper and silver ions. Check this link for more info.
Malassezia furfur is a unicellular organism with a dimater of 2.0-6.5 micrometers.
What is the best treatment for fungal acne, according to dermatologists?
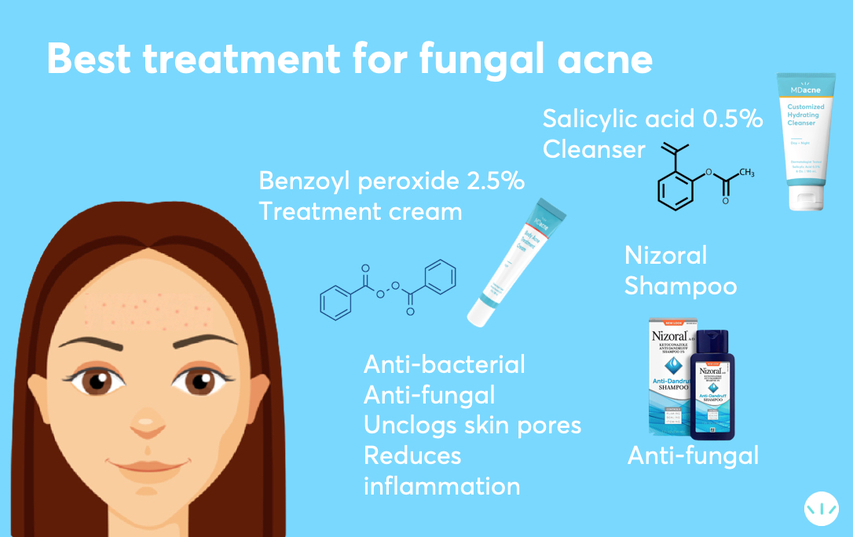
Fungal acne can be stubborn and difficult to treat—if you don't use the right fungal acne products! That being said, by implementing a good fungal acne skincare routine with the right topical treatments, including anti-fungal medications and targetted acne medications, it is possible to treat fungal acne effectively and very quickly.
- Anti-Fungal Shampoo/Body Wash: The best fungal acne treatment shampoos contain ketoconazole 2% (AKA, the anti-dandruff shampoo, Nizoral). While they are often called "shampoos," they can treat yeast infections in the hair and the face, and body. Use this every other day for at least two months for optimal results. Leave the solution on your skin for about 3-5 minutes and rinse it off. After the fungal acne is cleared, one should continue to use this shampoo once a week for at least three additional months to prevent relapse.
Prescription: because ketoconazole cream 2% is only available as a prescription, we recommend you consult your dermatologist or family physician to get a prescription right away.
Over-the-counter: if seeing a doctor is not an option, you can try Nizoral A-D with ketoconazole 1%. You can also try other dandruff shampoos Selsun Blue and Head and Shoulders.
--> Note: Some Dermatologists recommend shampoos with Zinc Pyrithione (heads and shoulders). Although Zinc Pyrithione is a mild anti-fungal and keratolytic agent, studies have shown that it's less effective than ketoconazole at inhibiting Malassezia. - Medicated Acne Cleanser: A medical-grade cleanser with salicylic acid and green tea extract will help unclog the skin pores and significantly increase Nizoral shampoo's effect on fungal acne. Use this on alternating nights with your anti-fungal shampoo.
- The best Acne Treatment Cream for fungal acne on the face: To eliminate fungal acne fast, there is a need to unclog the skin pores and fight both yeast and any harmful skin bacteria. To tackle your fungal acne (and any other acne) you have fast, consider adding a nighttime acne treatment cream with salicylic acid (BHA) or benzoyl peroxide. Combined with your two cleansers, this cream will help remove and destroy both the bacteria (acne vulgaris) and fungus on contact. Benzoyl peroxide is the best single ingredient (antimicrobial) to fight both acne bacteria and yeast. Salicylic acid is a keratolytic and has anti-inflammatory, antibacterial, and anti-fungal properties. It's an oil-soluble hydroxy acid meaning it does a great job of dissolving all the fungi that accumulate inside clogged pores.
--> to find the right medicated treatment (+ cleanser and moisturizer) cream for your skin, take the free MDacne skin analysis. - The best Acne Treatment Cream for fungal acne on the body: The body's skin is thicker and can tolerate a more potent treatment than the face. The best way to fight fungal acne on the body will be with creams that include both benzoyl peroxide 5% and tea tree oil. The benzoyl peroxide will destroy both the bacteria (acne vulgaris) and fungi on contact, and the tea tree oil with help reduce inflammation and eliminate the fungus. An excellent example of a body cleanser and body anti-acne treatment kit is the MDacne body acne treatment Duo.
- Oil-free Moisturizer: It's essential to moisturize your skin with fungal acne with a fungal acne-safe moisturizer. This is especially important when using the potent, medicated products above, causing some initial dryness and irritation (on top of the already itchy fungal acne!). However, make sure you are using an oil-free moisturizer so that you're not providing the yeast with even more of their favorite food!
- Hygiene: Make sure you wear clean clothes every day. When exercising, change out of any sweaty clothes ASAP and wipe down with an oil-free wipe until you can properly cleanse in the shower.
- Diet: Sticking to a proper diet can be a good addition to your fungal acne skincare routine. Consider reducing your sugar intake for some time—including high-sugar fruits and simple carbs that break down quickly into sugar—until your skin condition has improved.
- How long does it take to get rid of fungal acne?
Can covid masks cause more fungal acne?
Yes, they do. The best environment for fungi is humid, warm places. The mask's area acts as an incubator, providing the best environment for the skin fungi to flourish and cause acne breakouts under the mask. The fungi that accumulate on the skin under the mask and in the hair follicles clog the skin pores and trigger redness and inflammation.
The single-use surgical masks, made of plastic and other synthetic cloth masks, increase the heat and humidity in the moist environment under the masks and increases the risk for maskne.
Using antibiotics to treat pimples under the mask can paradoxically crease the risk for fungal maskne. Topical antibiotics such as erythromycin or clindamycin and oral antibiotics minocycline and doxycycline destroy the bacteria allowing fungi to overgrow and take their place.
How to differentiate regular bacterial maskne from fungal maskne?
Like other places on the face, fugal maskne will usually manifest as tiny, identical, itchy red bumps. In contrast, regular bacterial maskne will usually be made of groups of different types, different sizes of non-itching pimples.
How to prevent and treat fungal maskne?
Everybody needs to use a covid mask. That said, the type of mask is important.
The best prevention of fungal acne would be using cotton masks that are preferably infused with anti-fungal copper and silver. The treatment should include a gentle cleanser that has anti-fungal effects.
Cleansers with salicylic acid and green tea extract can be helpful and are readily available. Same as with other types of fungal acne, the use of Nizoral shampoo every other day is expected to be an excellent addition to your skincare routine.
The best over-the-counter treatment creams for maskne contain benzoyl peroxide and salicylic acid that are anti-bacterial and anti-fungal. Topical or antibiotics should be avoided.
Fungal acne/folliculitis can last for many weeks, months, or even years if not treated correctly. If treated with the right products, it can begin clear in as little as a few days, with significant improvement in just a matter of weeks. More severe cases may take longer but typically do respond with these same treatments.
How to use Nizoral for fungal acne?
Fungal acne, aka pityrosporum folliculitis, is caused by the same fungus that causes dandruff. If you're struggling with acne does not seem to budge using products marketed to treat acne, you should look for fungal products like Nizoral. Nizoral shampoo is based on an anti-fungal medication called ketoconazole. It reduces fungus levels on the skin and is commonly used to treat dandruff pimples when resistant to other therapies. Nizoral treats fungal infections, reduces the overgrowth of fungi on the skin, and prevents fungal acne.
You can use Nizoral shampoo every day, or every other day, for three weeks. Use it as a liquid cleanser. Leave it on the skin for it to do its job, so you should apply, lather, and count to 30 before rinsing off.
For how long should you use Nizoral for fungal acne?
You should see a reduction of your fungal acne for people with fungal acne in 3-4 weeks. Once your fungal acne clears up, use it twice weekly for maintenance for a few more months.
Can I combine Nizoral shampoo with other treatments?
Nizoral shampoo works great with salicylic acid, a beta-hydroxy acid that helps reduce oil production and dead cells from the skin to keep the pores clear.
What not to do when you have fungal acne?
For optimal results, avoid oily moisturizers and avoid topical antibiotics. Avoid using coconut oil and olive oil on your scalp and hair can cause forehead acne.
Are there any other benefits of using Nizoral shampoo?
Nizoral is a dandruff treatment shampoo. If you have dry, flaky skin on your scalp, Nizoral may help. People with Athlete's foot can benefit from using Nizoral once or twice daily use of Nizoral—be sure to dry any treated areas well, as fungus thrives in warm, humid areas.
Are there any side effects of Nizoral?
Using Nizoral shampoo is usually very safe. In rare cases, people who use normal can experience some itching or an allergic rash in the treatment area; pregnant and breastfeeding women should avoid Nizoral.
Does tea tree oil help treat fungal acne?
Multiple studies have shown that tea tree oil (AKA Melaleuca alternifolia) has strong anti-fungal properties—particularly against Malassezia, the main culprit in fungal acne. Tea tree oil should be combined with salicylic acid or benzoyl peroxide to penetrate the clogged skin pores. The best products to fight fungal acne on the face should be oil-free (not feed the fungi with oil) and contain both benzoyl peroxide and tea tree oil. In severe cases of fungal acne/folliculitis, there is a need to use oral anti-fungal tablets such as fluconazole.
The best COVID face masks for people with regular and fungal acne
References:
Malassezia (Pityrosporum) Folliculitis
Pityrosporum folliculitis: diagnosis and management in six female adolescents with acne vulgaris
Steroid acne vs. Pityrosporum folliculitis: the incidence of Pityrosporum ovale and the effect of anti-fungal drugs in steroid acne
Differential diagnosis of facial acne on black skin.
Microorganisms inhabiting follicular contents of facial acne are not only Propionibacterium but also Malassezia spp.
To find the right acne treatments for your unique skin, take the free skin assessment by clicking here.
How Long Does It Take For Fungal Acne To Clear
Source: https://www.mdacne.com/article/fungal-acne-causes-and-treatments-according-to-dermatologists
Posted by: harrwalwascalith.blogspot.com


0 Response to "How Long Does It Take For Fungal Acne To Clear"
Post a Comment